After the introduction of spiral CT in 1990, wide detector CT in 2004, Dual Source CT in 2005 and Dual Layer CT detectors in 2013, computed tomography is a mature modality that has reached a saturation phase. Despite technological progress, limitations remain for current CT technology.
With photon-counting CT, we have developed a radically new technology for clinical routine. At its core is a new kind of detector that is substantially different from a standard energy integrating detector.
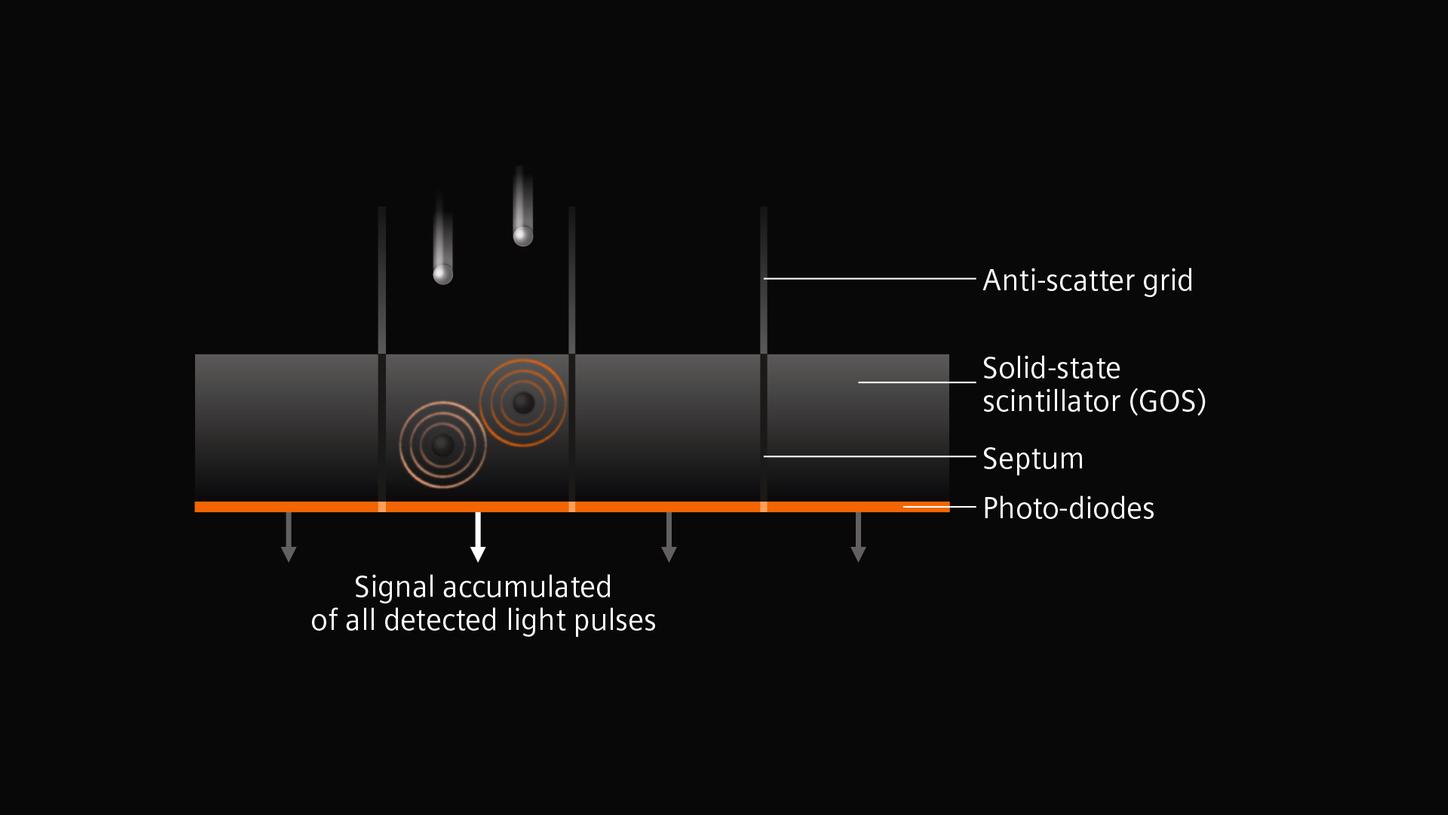
Watch the animation for an explanation of how the technology behind these photon-counting detectors work and how they could overcome the limitations of current CT detectors by providing CT data at high spatial resolution, without electronic noise, with improved contrast-to-noise ratio, at lower radiation dose and with intrinsic spectral information.